Introduction:The body mass index (BMI) and geriatric nutritional risk index (GNRI) are nutrition-related risk assessment tool and has been used in various clinical settings. The relationship between BMI and the associated risk of hematopoietic stem cell transplantation (HSCT), such as relapse and non-relapse mortality (NRM), have been reported (Fuji S et al. BMT. 2014;49:1505). However, the relationship between GNRI and HSCT outcome remains inconclusive. We aimed to evaluate the association between GNRI and overall survival (OS), relapse, and NRM of patients who received allogenic HSCT for hematological malignancies.
Methods:We retrospectively analyzed aged 16 years or older patients who underwent first allogeneic HSCT from January 2010 to December 2022 at the Jikei university hospital. The primary endpoints of this study was OS at 5 years. Secondary endpoints were NRM, the incidences of relapse, all-grade acute GVHD and chronic GVHD. Nutritional risk was evaluated both BMI and GNRI. Patients were classified into three groups based on pre-transplant BMI (underweight; BMI <18.5, overweight; BMI ≥25, and others as standard), and also classified into three groups based on pre-transplant GNRI (low-risk; GNRI>98, intermediate-risk; 92≤GNR≤98, and high-risk; GNR<92). GNRI was calculated as follows: (1.519 x serum albumin) + (41.7 x current body weight/ ideal body weight). Data on serum albumin level and body weight were collected at the beginning of conditioning regimen.
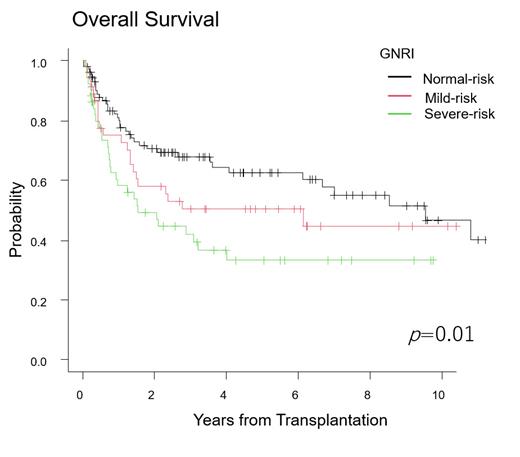
Results:Two hundred and three patients who received allogeneic HSCT for hematological malignancies (acute myeloid leukemia; n=98, acute lymphoblastic leukemia; n=51, myelodysplastic syndrome; n=27, myeloproliferative neoplasms; n=8, chronic myeloid leukemia; n=18, and other leukemias; n=2) were evaluated. The median age was 52 years old (range 16-69). The median follow-up period of survivors was 1394 days (range 51-4420) after allogeneic HSCT. The donor sources consisted of 39 (19.2%) HLA-matched related donor, 50(24.6%) HLA-mismatched related donor, 26(12.8%) HLA-matched unrelated donor and 88(43.4%) HLA-mismatched unrelated donor. One hundred and nine patients (53.7%) received myeloablative conditioning regimens. Based on the BMI, underweight, standard, overweight were included 33 (16.3%), 139 (68.4%), and 31 (15.3%) patients, respectively. While, based on the GNRI, the low-risk, intermediate-risk and high-risk were divided into 105 (51.7%), 46 (22.8%), and 51 (25.2%) patients, respectively . The 5-year OS rates of standard, underweight, and overweight were 52.6%, 39.5%, and 62.1%, respectively (p=0.07). On the other hand, the 5-year OS of low-risk, intermediate-risk, and high-risk were 62.6%, 50.4%, and 33.2%, respectively (p=0.01). In addition, multivariate analysis showed high-risk group showed significantly lower OS (p=0.03). Five-year cumulative incidences (CI) of relapse in the standard, underweight, and overweight, were 46.4%, 45.4%, and 25.0%, respectively (p=0.11). However, multivariate analysis showed that CI of relapse ratio was significantly lower in overweight group (p=0.02). While, 5-year CI of relapse rates in the low-risk, intermediate-risk, and high-risk were 36.5%, 47.2%, and 52.5%, respectively (p=0.03). However, multivariate analysis showed that there were no significant differences in relapse among three risk groups (p=0.06). There were no significant differences in CI of NRM, acute GVHD and chronic GVHD either BMI or GNRI. Subgroup analysis in the patients who underwent HSCT in complete remission revealed that there was no significant difference in OS among the three BMI groups (p=0.11), as well as the three GNRI groups (p=0.06). For the patients in non-remission at the time of allogeneic HSCT, there was no significant difference in OS between the three groups in BMI; however, OS was shorter in the high-risk group in GNRI (p=0.01).
Conclusions:In our study, OS of high-risk group defined by GNRI showed significantly poor , especially in non-remission patients. Although overweight defined by BMI did predict low CI of relapse, overweight did not predict OS. These results suggest that nutrition-related risk assessed by GNRI could be prognostic marker for survival in patients who received allogeneic HSCT.
Disclosures
Yano:Otsuka Pharmaceutical: Research Funding; Astra Zeneca: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal